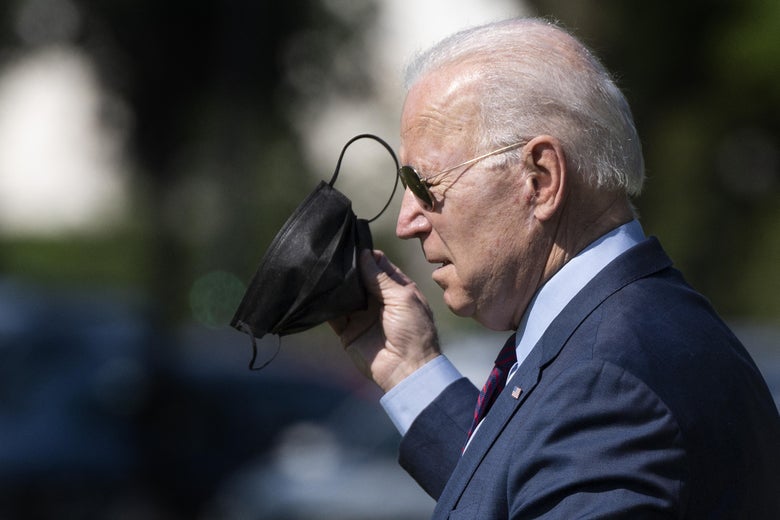
Last week, the Centers for Disease Control and Prevention surprised everyone by announcing updated guidance about COVID-19 precautions. Fully vaccinated people no longer have to wear masks or maintain 6 feet of distance in most indoor environments. The science underlying the recommendation that vaccinated people can take off their masks is very solid, but the way it’s being communicated is anything but. There was little prior notice of this change, and while reactions have been decidedly mixed, most of the dialogue concerns the many questions that have yet to be answered to the satisfaction of the public.
Why such a profound shift in recommendations and why now? Top health officials emphasized that this decision is supported by a rapidly growing body of scientific evidence. We know from animal studies, clinical trials, and, increasingly, from real-world data that the vaccines provide exceptional protection against symptomatic COVID-19. Vaccinated people are not likely to get sick if they are exposed, so the data does strongly support that it is safe for fully vaccinated people to remove their masks.
When the vaccines were first authorized, the clinical trials showed high efficacy at preventing symptomatic disease, but it wasn’t clear whether they would also prevent infection. Clinical trials were designed to assess protection against the disease COVID-19, but investigating the vaccines’ abilities to block infection altogether had to wait until vaccines were rolled out into the population. From real-world studies done in the U.S., the U.K., Israel, and Denmark, we now have the answer to that: They are very effective at preventing infection in the majority of those vaccinated, with the exception of older people and those who are immune compromised. In studies of vaccinated health care workers in Israel, Texas, Minnesota, and California, vaccines were exceptionally protective against infection even in the face of rising community transmission. The vaccines clearly can prevent many infections, which at population level will mean reductions in transmission, since people cannot spread SARS-CoV-2 to others if they are not infected to begin with.
But what about those who are infected despite being fully vaccinated? The CDC’s announcement coincided with a cluster of breakthrough infections among fully vaccinated members of the New York Yankees, spurring fresh concerns about whether breakthrough infections can be transmitted to others, including other vaccinated people. There is lean data on transmission by vaccinated people, although a study from the U.K. suggests that, like most of the cases among the Yankees, breakthrough infections usually appear to be asymptomatic and not associated with household spread. Furthermore, breakthrough infections were found to be associated with much lower viral loads than in unvaccinated people, which in turn are associated with reduced transmission. In other words, most vaccinated people who do get infected are not shedding enough infectious virus to spread it efficiently to others. This also might explain why breakthrough infections are frequently asymptomatic: Their vaccinated immune systems are rapidly and robustly responding to clear the infection, so there is no clinical disease and very little virus shedding.
Finally, the guidance is also based on sustained declines in new cases. At the peak of the winter surge in early January, the rolling seven-day average of new cases reported to CDC exceeded 250,000 new cases per day. As of May 15, that number has dropped to about 32,000.
While this is good news, it also is one of the biggest causes of concern around lifting this guidance now. These national averages can disguise the fact that prevalence and immunization rates vary substantially by region and community. Many are worried that communities with low vaccination rates are vulnerable to resurgence, especially where new cases have plateaued and are not continuing to decline. The CDC’s new mask guidance makes more sense in San Francisco, where COVID prevalence is extremely low and the majority of residents have been fully vaccinated, compared with Sacramento, where prevalence is about three times higher and only about 35 percent of residents have been fully vaccinated. If the CDC had waited, or linked this guidance to benchmarks at the county or state level, it could have avoided shifting the burden to the behavior of individual people. Because it released this blanket guidance now, without accounting for the local discrepancies in community risk, the most crucial question then becomes not whether the guidelines are evidence-based, but whether or not people will comply with them.
Unfortunately, things do not look promising so far. Though the CDC cites a Harris poll finding that most Americans understood previous mask recommendations and planned to abide by them, it’s not clear that applies to this guidance, or extends to resulting policy decisions and individual behavior. Within several days of the announcement, 18 states and many businesses announced an end to mask mandates for fully vaccinated people. With no infrastructure in place to verify a person’s vaccination status, this is based entirely on the honor system, which only goes so far. Already, social media has filled with anecdotal reports of people misrepresenting either their own vaccine status or the guidance itself, including a viral video of actor Ricky Schroder aggressively confronting a Costco employee about the chain’s continued masking requirements. It’s unclear whether Schroder is vaccinated, but as his apology included statements about “independence from medical tyranny,” it certainly seems plausible that he is not.
In theory, the guidance is supposed to incentivize vaccination, and the opportunity to resume a mask-free life will certainly be a strong inducement for some. But the CDC’s guidance seems to assume that anyone over the age of 12 who wants to be vaccinated can do so immediately. But major disparities in vaccine access remain, leaving millions behind. Some workers cannot take time off to get to an immunization site or fear they will have side effects without sick leave. People who are homebound or who don’t have ready access to transportation struggle to get to a vaccination site. Many states still require navigating a byzantine system to book an appointment, and vaccines are still not available in the offices of primary care providers. These barriers to access disproportionately affect racially and socioeconomically marginalized communities. Black and Hispanic communities have the lowest proportion of people vaccinated, and it is not because these communities are more vaccine-hesitant than others; it is because of limited access. Overall, many states just started offering vaccines to all this month, meaning there simply isn’t enough time for a majority to be fully vaccinated. Children under the age of 12 will not be eligible for vaccination until at least next year.
To a degree, the CDC is in a no-win situation. Many public health pundits who previously chided the CDC for being too timid and issuing guidance that was too complicated now complain that the agency’s recommendations were premature and the updated guidance was not complex enough. Any CDC action or lack thereof will be viewed as insufficient by a large number of people. Move too slowly, and it is accused of being too conservative, while drastic changes are criticized as reactionary and unjustified. At the same time, public trust in the CDC and governmental health agencies has sharply eroded, with a recent poll showing that only half of Americans have a great deal of trust in the CDC. It is imperative that public health agencies do everything in their power to rebuild that lost trust. A surprise announcement of radical changes does not reassure people, and even pointing to the science does little to answer questions about why this was the best decision now, given that some communities are much more vulnerable than others.
Whatever the scientific case, the public deserves insight into how and why public health guidance is issued. Even when recommendations are backed by strong scientific data, analysis of the evidence and formulation of public recommendations must be more transparent, particularly when the success or failure depends on public compliance with guidelines. Public health necessarily demands the engagement and participation of the public. Going forward, our public health leaders must do better to make sure they have this before pressing ahead with guidelines that are so fundamental to our daily lives and our health and safety.
Future Tense is a partnership of Slate, New America, and Arizona State University that examines emerging technologies, public policy, and society.
"now" - Google News
May 18, 2021 at 10:03PM
https://ift.tt/3oyOZ9N
Why Did the CDC Change Its Mask Guidance Now? - Slate
"now" - Google News
https://ift.tt/35sfxPY
Bagikan Berita Ini















0 Response to "Why Did the CDC Change Its Mask Guidance Now? - Slate"
Post a Comment